- Perform Kegel exercises to strengthen pelvic muscles and support the weakened fascia.
- Avoid constipation by eating high-fiber foods and drinking plenty of fluids.
- Avoid bearing down to move your bowels.
- Avoid heavy lifting.
- Control coughing.
- Lose weight if you're overweight or obese.
Procedures
You can usually fix a prolapsed uterus with medications, home care, or surgery. Uterine prolapse is when the uterus sags through the pelvic muscles that usually keep it in place.
Self-care
Surgery can involve: Repair of weakened pelvic floor tissues. This surgery is generally approached through the vagina but sometimes through the abdomen. Removal of your uterus (hysterectomy). Hysterectomy might be recommended if uterine prolapse is severe.
Nutrition
Your doctor will perform uterine prolapse surgery using one of the following approaches: Minimally invasive surgery uses a laparoscope, which is a thin, lighted instrument with a small camera that transmits pictures of the inside of your body to a video screen.
Can you fix a prolapsed uterus?
Kegel exercises. Kegel exercises strengthen your pelvic floor muscles. A strong pelvic floor provides better support for your pelvic organs, prevents prolapse from worsening and relieves symptoms associated with uterine prolapse.
How do you fix pelvic floor prolapse?
How is uterine prolapse surgery performed?
What are the best exercises for uterine prolapse?
See more

How do you fix uterine prolapse?
Treatment for uterine prolapse includes lifestyle changes, a pessary, or surgery to remove the uterus. You may be able to prevent this condition with weight loss, a high fiber diet, not smoking, and doing Kegel exercises.
Can I reverse my uterine prolapse?
The bottom line In some cases, it's possible to ease symptoms or reverse a mild uterine prolapse by doing pelvic muscle exercises, along with other self-care measures. Prolapsed uterus doesn't always require other treatment. But in severe cases, use of a vaginal pessary can provide the necessary support.
Can a prolapse be fixed without surgery?
The two non-surgical options for prolapse are pelvic floor muscle training (PFMT) and a vaginal pessary. PFMT can be effective for mild prolapse but is usually not successful for moderate and advanced prolapse. The main alternative to surgery for prolapse is a vaginal pessary.
Can you fix a prolapse on your own?
Kegel exercises can help to strengthen your pelvic floor muscles. When you have pelvic organ prolapse, your pelvic organs -- your bladder, uterus, and rectum -- are weak. They can drop down toward your vagina. Kegels can help make those muscles stronger and keep your prolapse from getting worse.
Can I push my prolapse back up?
If you have a rectal prolapse, you may be able to push the prolapse back into place as soon as it occurs. Your doctor will let you know if this is okay to do. Put on disposable gloves, and put lubricating jelly on your finger. Gently push back any tissue that has come out of the anus.
How do you fix a prolapsed uterus naturally?
You could try to:Perform Kegel exercises to strengthen pelvic muscles and support the weakened fascia.Avoid constipation by eating high-fiber foods and drinking plenty of fluids.Avoid bearing down to move your bowels.Avoid heavy lifting.Control coughing.Lose weight if you're overweight or obese.
Can you live with a prolapsed uterus?
It can be the womb (uterus), bowel, bladder or top of the vagina. A prolapse is not life threatening, but it can cause pain and discomfort. Symptoms can usually be improved with pelvic floor exercises and lifestyle changes, but sometimes medical treatment is needed.
What happens if prolapse is left untreated?
If prolapse is left untreated, over time it may stay the same or slowly get worse. In rare cases, severe prolapse can cause obstruction of the kidneys or urinary retention (inability to pass urine). This may lead to kidney damage or infection.
Can you heal a prolapse naturally?
Uterine prolapse treatment Prolapse up to the third degree may spontaneously resolve. More severe cases may require medical treatment. Options include vaginal pessary and surgery.
How do I know if my prolapse is severe?
Signs and symptoms of moderate to severe uterine prolapse include:Sensation of heaviness or pulling in your pelvis.Tissue protruding from your vagina.Urinary problems, such as urine leakage (incontinence) or urine retention.Trouble having a bowel movement.More items...•
Is walking good for prolapse?
What type of exercise is best for pelvic organ prolapse? Aerobic exercises three to five times a week (walking, cycling, swimming etc). Aerobic exercise helps your cardiovascular system, muscles, tendons and ligaments to stay strong and will also help you maintain to the correct weight (BMI) for your height and age.
How do I know what kind of prolapse I have?
How prolapse is named depends on which organ is affected:Cystocele is when the bladder protrudes into the vagina, creating a bulge. It's the most common form of prolapse.Rectocele is when the rectum bulges into the back wall of the vagina.Uterine prolapse involves the uterus dropping into the vagina.
Can a Stage 2 uterine prolapse be reversed?
Can Pelvic Prolapse be Reversed? Yes! Pelvic organ prolapse can be treated and improve without surgery in some women. Prolapse results when the pelvic floor tissues are overstretched and weakened, just like overstretching a spring.
How do I put my uterus back in place?
Exercise: Special exercises, called Kegel exercises, can help strengthen the pelvic floor muscles. This may be the only treatment needed in mild cases of uterine prolapse. To do Kegel exercises, tighten your pelvic muscles as if you are trying to hold back urine.
Can Kegels reverse mild prolapse?
In the journals: Pelvic floor muscle training can help reverse pelvic organ prolapse. Pelvic floor strengthening exercises, also known as Kegel exercises, are known to be effective for stress urinary incontinence in women, with cure rates of up to 80%.
Is walking good for prolapsed uterus?
What type of exercise is best for pelvic organ prolapse? Aerobic exercises three to five times a week (walking, cycling, swimming etc). Aerobic exercise helps your cardiovascular system, muscles, tendons and ligaments to stay strong and will also help you maintain to the correct weight (BMI) for your height and age.
How do you treat uterine prolapse?
Some more severe cases of uterine prolapse require surgery. Doctors often perform the surgery laparoscopically, where they insert instruments through the navel. They may also go through an abdominal incision. In both cases, they pull the uterus back into place, reattaching the ligaments for support.
Who gets a prolapsed uterus?
Women who give birth — especially vaginally — are at the highest risk of experiencing uterine prolapse. Other risk factors include:
Why do women wait until they have children to have surgery to repair a prolapsed uterus?
Experts recommend that women wait until they are done having children to have surgery to repair a prolapsed uterus, because it is likely that giving birth again will cause another prolapse.
What is the American College of Obstetricians and Gynecologists's "Surgery for?
American College of Obstetricians and Gynecologists: "Surgery for Pelvic Organ Prolapse."
Is surgery for a prolapsed uterus risky?
Any surgery carries risks, including the surgery for a prolapsed uterus. Surgery may be riskier for you if you:
Is pelvic floor exercise dangerous?
Doing pelvic floor exercises and using a pessary are low-risk. However, doing either of these outside of the care of a doctor may be dangerous. You should get proper training on how to perform the exercises and use a pessary to avoid further injury.
Is uterine cancer fatal?
Uterine cancer is not fatal when it is diagnosed and treated in the early stages. Generally, a 5-year survival rate for patients in stage 1 of uterine cancer is 90%. However, the 5-year survival rate can vary depending on the extent to which the cancer has spread.
What is the result of a pelvic organ prolapse?
In some cases, frank protrusion of these organs can occur. Pelvic organ prolapse can result in symptoms including urinary leakage, constipation, and difficulty with intercourse.
What is a laparoscopic colposuspension?
Laparoscopic colposuspension is a minimally invasive surgical technique that provides a safe and durable method for reconstruction of the pelvic floor and its contents without the need for a large abdominal incision.
How is colposuspension performed?
Laparoscopic colposuspension is performed through 4 small keyhole (0.5-1 cm) incisions across the mid abdomen (Figure 1). Through these small incisions, fine laparoscopic instruments are inserted to dissect and suture. Excellent visualization of the pelvic organs is achieved with the use of a high-powered telescopic lens attached to a camera device, which is inserted into one of the keyhole incisions.
What is a fistula in the vagina?
Vesicovaginal fistula: A fistula (abnormal connection) between the bladder and vagina is a rare complication of any pelvic surgery involving the vagina , uterus, and bladder. A vesicovaginal fistula typically manifests with symptoms of continuous urinary leakage from the vagina.
How long does colposuspension take?
The length of operative time for laparoscopic colposuspension can vary greatly (3-5 hours) from patient to patient depending on the internal anatomy, shape of the pelvis, weight of the patient, and presence of scarring or inflammation in the pelvis due to infection or prior abdominal/pelvic surgery.
Why do you have to convert to open surgery?
Conversion to Open Surgery: The surgical procedure may require conversion to the standard open operation if extreme difficulty is encountered during the laparoscopic procedure (e.g. excess scarring or bleeding). This could result in a standard open incision and possibly a longer recuperation period.
Is colposuspension safe?
Although laparoscopic colposuspension has proven to be very safe, as in any surgical procedure there are risks and potential complications. Potential risks include:
How to treat a prolapsed vagina?
1. Know that vaginal surgery is the mainstay of treatment for more severe vaginal prolapse. While strategies such as activity modification, pessaries, Kegel exercises, and estrogen replacement therapy can be helpful, moderate to severe cases of vaginal prolapse may need to be treated with surgery.
What to do when you have a prolapse?
As you await surgery, you may be offered treatments such as a vaginal pessary to help control your prolapse until it can be corrected surgically.
What exercises strengthen pelvic floor muscles?
Perform Kegel exercises to strengthen your pelvic floor muscles. [5]
Why does my vagina prolapse after menopause?
Many cases of vaginal prolapse occur following menopause. They are linked to the decreased estrogen that is present post-menopause, as a decreased estrogen level correlates to a weakening of the vaginal area and the surrounding muscles and ligaments.
How to identify pelvic muscles?
To identify your pelvic muscles (the ones you will be flexing during Kegel exercises), stop urinating mid-stream. Notice which muscles you used to do this task - this feeling of muscle tightening is what you will be aiming for when you perform the exercises (which is recommended to do when you are not urinating - the urination test is simply used to allow you to identify the muscles).
Why does my vagina prolapse?
Vaginal prolapse can occur when the muscles and ligaments in your pelvis become weakened, result ing in tissue that protrudes from your vagina because it is unable to be properly held in place. Needless to say, having a vaginal prolapse can be a significant concern, both cosmetically and functionally. If your vaginal prolapse is mild, you may be ...
How to prevent vaginal prolapse?
Change your activities to prevent stress to the vaginal walls. If you have only mild vaginal prolapse, your doctor will likely recommend modifying your activities to avoid heavy lifting and/or straining. This will reduce the stress on your pelvic floor muscles, and may help to improve (or at least to prevent worsening of) your vaginal prolapse.
How to prevent uterine prolapse?
There is no definitive way to prevent uterine prolapse. Losing weight, eating a fiber-rich diet, quitting smoking and performing pelvic floor exercises can help to reduce the risk of this condition.
What causes uterine prolapse?
Uterine prolapse is caused when the muscles and tissue of the pelvic floor are weakened and can’t support the weight of the uterus. This lets it drop into your vagina.
How is uterine prolapse diagnosed?
If your healthcare provider thinks that you have a prolapsed uterus, he or she will probably do a physical exam to check your pelvis. If you also have urinary incontinence or a feel like you can’t empty your bladder, your doctor may do a procedure called a cystoscopy to examine your bladder and urethra.
What is the difference between a pessary and a hysterectomy?
A pessary can also relieve symptoms. This is a device your healthcare provider inserts into your vagina to support your pelvic organs. A hysterectomy is a surgery to remove your uterus. This can be done through your vagina. The healing time is faster than with surgery that requires an abdominal incision.
What causes a woman's uterus to prolapse?
When pelvic muscle, tissue and ligaments weaken, the uterus can drop down into the vaginal canal, causing uterine prolapse. Nearly one-half of all women between ages 50 and 79 have some degree of uterine or vaginal vault prolapse, or some other form of pelvic organ prolapse. Factors that increase your risk of uterine prolapse include childbirth, ...
What does it mean when your uterus drops down?
Uterine prolapse occurs when the muscles and tissue in your pelvis weaken. The weakness lets the uterus drop down into your vagina. Sometimes, it comes out through your vaginal opening. Nearly half of all women between ages 50 and 79 have this condition.
How to treat a coughing pelvic organ?
Seek prompt treatment for a chronic cough, which can place extra pressure on your pelvic organs. Do Kegel exercises to strengthen your pelvic floor muscles. These actions may also help if you already have uterine prolapse. See your healthcare provider when symptoms first start to bother you.
How to repair a prolapsed uterus?
Surgery: Surgical repair of a prolapsed uterus can be performed through the vagina or abdomen. It involves skin grafting, or using donor tissue or other material to provide uterine suspension. A hysterectomy may be recommended.
What causes a uterus to prolapse?
Treatment. Exercises. A uterine prolapse is when the uterus descends toward or into the vagina. It happens when the pelvic floor muscles and ligaments become weak and are no longer able to support the uterus. In some cases, the uterus can protrude from the vaginal opening. Complications can sometimes result, including ulceration ...
What is a vaginal pessary?
Vaginal pessary: This is a vaginal device that supports the uterus and keeps it in position. It is important to follow the instructions on care, removal, and insertion of the pessary. In cases of severe prolapse, a pessary can cause irritation, ulceration, and sexual problems.
Why do my pelvic muscles get weak?
Pelvic floor muscles can become weak for a number of reasons: pregnancy. factors related to delivery, including trauma, delivering a large baby, or having a vaginal delivery. getting older, especially after menopause, when levels of circulating estrogen drop. frequent heavy lifting. straining during bowel movements.
What are the problems with sex?
difficulties with sexual intercourse. urinary leakage, retention or bladder infections. bowel movement difficulties, such as constipation. lower back pain. uterine protrusion from the vaginal opening. sensations of sitting on a ball or that something is falling out of the vagina. weak vaginal tissue.
How is uterine uterus graded?
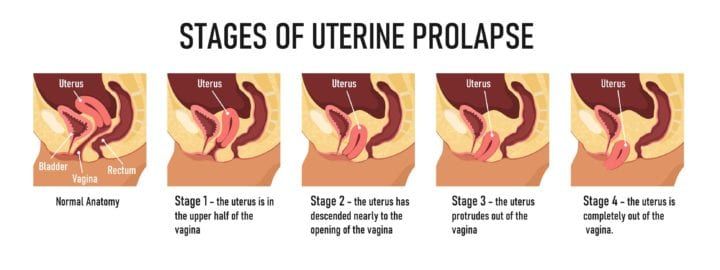
The condition is graded by its severity , determined by how far the uterus has descended: 3rd grade: cervix has descended outside the introitus. 4th grade: cervix and uterus have both descended outside the introitus. More severe cases may need surgery, but in the early stages, exercises may help.
What is the purpose of pelvic examination?
While examining the pelvis, the provider will evaluate for organ placement and vaginal tone.
How does a hysterectomy help a prolapsed uterus?
Hysterectomy helps treat a prolapsed uterus by removing it.
What is the procedure called when the uterus prolapses?
The types of uterine prolapse surgery include: Ligament suspension lifts the uterus using a mesh material or stitches to attach the uterus or vaginal vault (upper part of the vagina) to a strong ligament in the pelvis to support them. This is called a sacrospinous ligament suspension or uterosacral ligament suspension.
Who performs uterine prolapse surgery?
Obstetrician-gynecologists specialize in women’s health and pregnancy.
How does a vaginal approach work?
Vaginal approach involves repairing uterine prolapse through the vagina. Your surgeon inserts a speculum into the vagina to hold it open and repairs damage or weakness in the vaginal wall. This procedure does not require an incision into the abdomen and has a quicker recovery.
What is a prolapsed uterus?
Uterine prolapse surgery includes various procedures to repair a prolapsed uterus that has slipped out of place. This condition results from damage to or weakening of muscles, ligaments and tissues that hold a woman’s uterus in place. Uterine prolapse is more common in women who have had children. It can cause protrusion ...
What is the term for the ligament that attaches to the pelvis?
This is called a sacrospinous ligament suspension or uterosacral ligament suspension. Sometimes your surgeon lifts the uterus by attaching it to a muscle. This is called an ileococcygeus suspension. Uterine suspension lifts the uterus using a mesh material to attach the uterus to the pelvis.
What type of anesthesia is used for uterine prolapse surgery?
Types of anesthesia that may be used. Your doctor will perform uterine prolapse surgery using either general anesthesia or regional anesthesia. General anesthesia is a combination of intravenous (IV) medications and gases that put you in a deep sleep. You are unaware of the procedure and will not feel any pain.
What is pelvic organ prolapse repair?
These are repaired in several different ways, either conservatively, with non-surgical treatments or with surgery.
What is the procedure to repair a prolapsed bladder?
The type of surgical procedure conducted depends on the amount (degree) of prolapse and the location. Specific procedures include: Cystocele repair refers to the repair of the bladder prolapse. This can be done through a vaginal surgery and involves the reconstruction of the vaginal wall and tissue between the bladder and the vagina.
Why is synthetic mesh sometimes used in pelvic organ prolapse repair and what are the risks?
Understanding the conversation around transvaginal and synthetic mesh can be confusing.
What are the major risks associated with pelvic organ prolapse repair?
These may include excessive blood loss, an infection requiring antibiotic treatment, developing scar tissue, and childbirth complications.
What should I ask my doctor or OB-GYN if he/she recommends pelvic organ prolapse surgery?
Before undergoing surgery, you will likely have many questions for your doctor or OB-GYN. Below are some recommended questions to ask – and background information to help you weigh the answers. You can also download a printable version of these questions.
How DualPortGYN works?
Clearer view and fewer complications – DualPortGYN uses a technique known as retroperitoneal dissection (RPD), originally developed to remove cancerous tissue. By going behind (retro) the lining (peritoneal), the surgeon completely visualizes all of the anatomy of the pelvis, and avoids complications such as excessive bleeding, bladder injury, injury to the ureter and bladder. RPD allows surgeons to map the organs and arteries in the pelvis, much like a GPS system, reducing the time of the procedure and avoiding injury to the pelvic structures.
What have your other patients experienced after this procedure?
Robotic, open and conventional laparoscopic GYN surgeries can lead to longer recovery times, increased blood loss and larger scars than newer procedures. Make sure your surgeon is trained in the latest minimally invasive techniques, such as The Center for Innovative GYN Care’s DualPortGYN, that prevent injury to the pelvic structures and minimize blood loss – resulting in reduced complication rates and improved recovery times.
How to prevent uterine prolapse?
Kegel exercises and pelvic floor muscle training exercises are both easy exercises that can go a long way toward preventing the symptoms associated with uterine prolapse. Keep in mind that it is never too late to start strengthening your pelvic floor muscles with Kegel exercises .
What is the treatment for pelvic prolapse?
If a patient has slight or asymptomatic pelvic prolapse, the patient is recommended to engage in some type of non-surgical conservative therapy to quickly find a solution. Should the uterine prolapse be more severe, this is when physicians turn to something more permanent in the form of hysterectomies and surgical loops. [ 3 ]
What percentage of women have uterine prolapse?
Uterine prolapse is a condition that can affect up 50 percent of the female population at some point during life, and that can lead to a number of life-altering complications that can make it difficult for women to enjoy their years after menopause.
How many women have a prolapsed uterus?
Even if these women were educated on the risks and difficulties of having a prolapsed uterus, up to 70 percent of the population can have a prolapsed uterus (much higher than the epidemiology in the Western world).
Can you strengthen your uterine canal?
There are many natural and non-surgical interventions that patients can take to strengthen their uterine canals and find a solution for their uterine prolapse treatment. [ 2] Let's take a closer look!
Can Lajula root be used for uterine prolapse?
In the event that a trip to India is out of your price range, and you have a hard time getting your hands on this Lajula root extract, fear not, there are still plenty of non-surgical approaches to realize uterine prolapse treatment. These simple routines are very affordable and can go a long way in preventing more noticeable uterine prolapse symptoms.
Is uterine prolapse common?
A problem where uterine prolapse is quite extensive while management may be sparse takes us to developing countries like India, where uterine prolapse can be quite common and result in more extensive complications like urinary tract infections and even death.