- Drainage of the spilled fluid and food with chest tubes
- Endoscopy and stent placement (a hollow tube is placed in the esophagus to occlude the hole)
- Esophagectomy in extreme cases when the esophagus cannot be repaired
- Minimally invasive repair of the perforation site
- Open repair of the perforation
What are the symptoms of a perforated esophagus?
- Moderate or severe chest pain that may worsen upon breathing or swallowing following an episode of retching or vomiting.
- Fever.
- Rapid, shallow breathing, difficulty breathing (dyspnea)
- Excessive sweating.
- Subcutaneous emphysema.
- Abdominal or back pain.
- Difficulty swallowing (dysphagia)
What is the risk for perforation during esophageal dilation?
Two independent risk factors for development of perforation during dilation therapy for post-EMR/ESD stricture were identified: multiple dilations (odds ratio [OR] 1.2; P=0.012), and lower site of stricture (OR 12.8; P=0.043). Dysphagia was ameliorated by the dilations, and no patient required surgery.
What are potential complications of esophageal spasm?
trouble swallowing. heartburn. regurgitation of food or liquid back up into your mouth. Seek immediate medical care if you think you may be having an esophageal spasm. Given the severity of ...
What are the causes of esophageal atresia?
Up to half of all babies born with EA have one or more other birth defects, such as:
- trisomy 13, 18 or 21
- other digestive tract problems, such intestinal atresia or imperforate anus
- heart problems, such as ventricular septal defect, tetralogy of Fallot or patent ductus arteriosus
- kidney and urinary tract problems, such as horseshoe or polycystic kidney, absent kidney or hypospadias
- muscular or skeletal problems
- tethered spinal cord

How do you treat esophageal perforation?
Patients with perforation of the esophagus in a diseased esophagus are best treated by resection [8, 82]. Esophageal resection with or without immediate reconstruction should be considered for perforations in patients with megaesophagus, carcinoma, caustic ingestion, stenosis or severe undilatable reflux strictures.
How do they repair an esophageal tear?
Most people with a perforated esophagus do need surgery, especially if the hole is located in the chest or abdominal areas. During the procedure, your surgeon will remove scar tissue from the area around the perforation and then sew the hole shut.
Is esophageal perforation an emergency?
Esophageal perforation is a rare but frequently life-threatening condition that requires consideration in the appropriate clinical context in order to diagnose upon initial presentation. While the etiologies of this pathology are vast, by far most common is an iatrogenic cause, often secondary to endoscopic procedures.
Can esophagus be repaired?
The esophagus is a complex organ comprising nonredundant tissue that does not have the ability to regenerate. Hence, surgical repair and/or replacement of the esophagus are the only feasible treatment options upon extensive structural damage.
Can a perforated esophagus be repaired?
Surgery is often needed to repair a perforation in the middle or bottom portions of the esophagus. Depending on the extent of the problem, the leak may be treated by simple repair or by removing the esophagus.
How long does a damaged esophagus take to heal?
It might take 1 to 3 weeks to heal. Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor or nurse call line if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take.
What does an esophageal perforation feel like?
These include extreme chest pain, rapid heartbeat, shallow breathing, radiating shoulder pain, shortness of breath, and vomiting. If left untreated, esophageal tears can lead to sepsis, shock, and even death.
What happens if you get a tear in your esophagus?
The esophagus is the tube that connects the mouth with the stomach. When a tear occurs in this tube, the condition is known as esophageal rupture. A rupture allows food or fluids to leak into the chest and cause severe lung problems.
Is esophageal rupture rare?
Esophageal perforation is a rare and potentially life-threatening condition.
Can esophageal tear cause death?
Ruptures can be caused by surgical procedures, severe vomiting, or swallowing a large piece of food that becomes stuck in the esophagus, but some ruptures occur spontaneously. Symptoms include chest and abdominal pain, fever, and low blood pressure. Esophageal rupture can be fatal.
What is a esophageal perforation protocol?
This protocol is designed to aid in the management of identified or suspected esophageal perforations that can occur secondary to penetrating trauma; during esophageal, neck, or chest procedures; or are created by the placement of esophageal or endotracheal tubes. This is in contrast to the spontaneous esophageal rupture or Boerhaave's syndrome, as well as ruptures induced by tumor or foreign-body ingestion.
What should a patient do if an esophageal perforation is suspected at the time of?
If an esophageal perforation is suspected at the time of endoscopy, the patient should remain in the operating room and be evaluated by intraoperative exploration and endoscopy.
What procedures are needed for large perforations?
Large and extensive perforations could require drainage and diversion procedures , cervical esophagostomy, distal esophageal closure, and feeding gastrostomy or jejunostomy. Late repair or possible replacement procedures would follow.
When patients present late or have other complicating issues, a nonsurgical approach may be utilized if the perfor?
When patients present late or have other complicating issues a nonsurgical approach may be utilized if the perforation cavity is confined to the mediastinum and drains well into esophagus. These patients require close observation for progression of symptoms, frequent CXR, and normalized swallow studies prior to the initiation of PO intake.
How long does it take to get a full diet after a perforation?
After confirmed closure of perforation on repeat esophagram, begin a clear liquid diet and advance to full diet over 1 to 2 weeks.
How long should you be closely observed for perforation?
If no perforation is identified, the patient should be observed closely for at least 24 hours prior to the return of oral feeding with continued close observation. If the perforation is identified, then treatment plans are made and followed. TREATMENT. General.
What is the surgical management of well confined perforations?
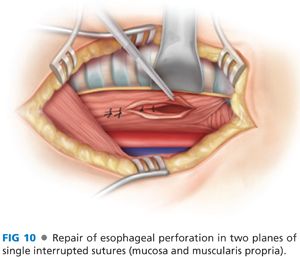
Surgery management for early well-confined perforations would consist of identification and debridement of nonviable tissue, followed by multilayered closure: mucosa, muscle, and then additional nearby tissues (pleura, pericardium, etc). This is followed by drainage and closure. Repeat radiology studies in 7 to 10 days if no signs of closure failure are identified in the interim.
What are the symptoms of cervical esophageal perforation?
In cervical esophageal perforation, patients often present with symptoms of neck pain, dysphagia, odynophagia, dysphonia, and subcutaneous emphysema. Symptoms of intrathoracic esophageal perforation are often more extreme and include chest pain, tachycardia, fever, leukocytosis, and hypotension. Intrathoracic esophageal perforation may rapidly contaminate the mediastinum, causing chemical irritation, inflammation, and sepsis. Chemical injury from the disrupted esophagus may cause the overlying pleura to rupture, and negative intrathoracic pressure draws saliva, gastric juice, and bacteria from the esophageal lumen into the pleural space, eventually leading to marked fluid shifts and shock.
How long does it take to repair esophageal perforation?
Successful outcomes for primary repair of esophageal perforation can be obtained even in delays in diagnosis greater than 24 hours. Wright and coworkers reported on 28 patients who underwent reinforced primary repair of thoracic esophageal injuries, with a total mortality of 14%.
What causes esophageal perforation?
Causes of esophageal perforation can be divided into instrumental and noninstrumental. Instrumental causes include endoscopy, both rigid and flexible, dilation of strictures or the esophagogastric junction (EGJ) by pneumatic balloon dilation or bouginage, and airway intubation. Noninstrumental causes include barogenic, penetrating, and operative trauma. The most common etiology of barogenic trauma is Boerhaave's syndrome. In 1723, Dr. Hermann Boerhaave detailed in his report, “History of a Grievous Disease Not Previously Described,” a postmortem on the Dutch admiral, Baron Jan Germit von Wassenaer.
What test is used to determine if a person has esophageal perforation?
Several diagnostic tests play important roles in identifying esophageal perforation. A chest radiograph should be obtained, looking for subcutaneous emphysema and pneumomediastinum. Contrast esophagography is the gold standard. Water-soluble gastrograffin should be avoided, as it is hypertonic and aspiration may lead to pneumonitis.
Where do esophageal perforations occur?
Although esophageal perforation may occur anywhere, certain types of esophageal injuries have a predilection to occurring at key anatomic areas. These areas correspond to natural points of narrowing, specifically, the criopharyngeus muscle of the cervical esophagus, the area of broncho-aortic constriction at the proximal one-third of the esophagus, and the distal EGJ ( Fig. 1 ). Iatrogenic cervical esophageal injuries, especially endoscopy, commonly occur at Killian's triangle, an area lacking posterior esophageal muscularis ( Fig. 2 ). This narrow area is bordered by the horizontal cricopharyngeus muscle inferiorly and the oblique inferior constrictor muscles superiorly. Ingested foreign bodies often become lodged at the broncho-aortic constriction, causing localized injury. Barogenic trauma occurs most frequently near the EGJ.
Where is the finger passed after esophageal repair?
Figure 8 After the esophageal repair, a finger is passed down posterior to the esophagus and anterior to the prevertebral fascia down into the superior mediastinum, followed by a sucker, to remove any fluid or effluent. A flat Blake drain is then placed into the superior mediastinum along this path and externalized, for closed drainage.
Which neck is best for cervical esophageal injuries?
The majority of cervical esophageal injuries should be approached via the left neck. The patient is placed in the supine position and a shoulder roll is placed beneath the scapulae to extend the neck, and the arms are tucked to the sides. The patient's head is rotated slightly to the right to provide optimal exposure of the left neck ( Fig. 3 ).
What is esophageal perforation?
Esophageal perforation. Perforation of the esophagus; Boerhaave syndrome. Share. An esophageal perforation is a hole in the esophagus. The esophagus is the tube food passes through as it goes from the mouth to the stomach. The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert ...
Why is there a hole in my esophagus?
Causes. When there is a hole in the esophagus, the contents of the esophagus can pass into the surrounding area in the chest (mediastinum). This often results in infection of the mediastinum ( mediastinitis ). The most common cause of an esophageal perforation is injury during a medical procedure. However, the use of flexible instruments has made ...
How long does it take for a stent to be placed in the esophagus?
If surgery is needed, it is best done within 24 hours. A stent may be placed in the esophagus if only a small amount of fluid has leaked. This may help avoid surgery. A perforation in the uppermost (neck region) part of the esophagus may heal by itself if you do not eat or drink for a period of time.
What causes esophageal surgery?
Trauma or injury to the chest and esophagus. Violent vomiting (Boerhaave syndrome) Less common causes include injuries to the esophagus area (blunt trauma) and injury to the esophagus during surgery ...
What to look for when you have a perforation in your esophagus?
Low blood pressure. Rapid heart rate. Neck pain or stiffness and air bubbles underneath the skin if the perforation is in the top part of the esophagus. You may have a chest x-ray to look for: Air in the soft tissues of the chest.
How to repair a perforated esophagus?
Surgery is often needed to repair a perforation in the middle or bottom portions of the esophagus. Depending on the extent of the problem, the leak may be treated by simple repair or by removing the esophagus.
How long does it take for Outlook to go away?
Outlook (Prognosis) The condition can progress to shock, or even death, if untreated. Outlook is good if the problem is found within 24 hours of it occurring. Most people survive when surgery is done within 24 hours. Survival rate goes down if you wait longer.
How to repair esophageal perforation?
Lesson 10. Transthoracic Repair of an Acute Esophageal Perforation 1 Observe the phenomenon of the submucosal/mucosal layer laceration extending for a greater distance proximally and distally than the muscular “laceration” and discuss why this is important to know 2 Learn the gentle handling of esophageal tissue. 3 Experience working through a low postero-lateral thoracotomy incision while repairing a distal esophageal perforation in a patient whose lung is being ventilated on the operative side.
How to extend a submucosal laceration?
Gently grasp with a forceps the proximal and distal ends of the “laceration” and extend the submucosal/mucosal “laceration” with Metzenbaum scissors 1 cm proximally and distally.
What is a goat mediastinal block?
Goat mediastinal tissue block. Fresh from local abattoir. Refrigera te. Consists of heart, lungs, esophagus, trachea, diaphragm, thoracic aorta and esophagogastric junction with attached proximal one third of the stomach.
What plane is the mannequin cut in half?
Mannequin of human chest (from local department or Men’s store) cut in half along the sagittal plane to create the simulation of a left hemi-thorax. Cut a wedge-shaped hole in lateral side of left chest mannequin to simulate a left postero-lateral thoracotomy incision.
Which muscle layer is tagged with two curved hemostats?
Two curved hemostats to “tag” sutures placed in esophageal muscle layer for exposure of submucosal layer.
What is lubricant tube?
Lubricant—tube of K-Y jelly or Lubriderm.
Why is early diagnosis and management important?
Early diagnosis and management is key to improved outcomes. Thus, it is important to appreciate those circumstances in which esophageal perforation might occur and to have a high index of suspicion in such instances.
How to insert loop wire in perforation?
For smaller holes, a loop wire can be inserted transthoracically through the perforation defect. Endoscopy is performed to retrieve the loop wire, which is then brought back through the mouth. The end of a T-tube is sutured to the loop wire, and the wire or T-tube is pulled transorally down the esophagus and out through the chest, with the T-tube tip positioned intraluminally at the perforation site. Final positioning of the T-tube can be confirmed by endoscopy.
What is replaced with scar tissue?
Damaged and destroyed esophageal submucosa and muscularis are replaced with scar tissue.
What is the best way to diagnose esophageal perforation?
Radiography is essential in the diagnosis of esophageal perforation.
What is the purpose of drainage, débridement, and control of the perforation site?
Drainage, débridement and control of the perforation site to prevent or treat sepsis.
Which side of the chest is perforated with dye?
Esophagram showing esophageal perforation with extravasation of dye into the right side of the chest.
How many percent of ingested foreign objects pass through the esophagus?
Usually, ingested foreign objects that are smaller than 2 cm pass through the normal adult esophagus without causing perforation. Eighty to ninety percent of ingested foreign objects pass through the esophagus and eventually the rest of the gastrointestinal tract without ...
How to treat a thoracic esophageal perforation?
Most thoracic esophageal perforations, especially spontaneous disruptions in ill or septic patients, are treated surgically with surgeons preferring primary surgical repair, surgical drainage, or esophageal resection. Early reviews,9–11however, have documented the successful nonoperative or conservative treatment of not only iatrogenic perforations but in those patients with Boerhaave syndrome or spontaneous perforation.13,14The major issues concerning the type of treatment of esophageal perforation as discussed by Cameron et al9are whether mediastinal contamination and/or free pleural fluid can be contained by chest tube drainage. These authors state that when the disruption is well drained, nonoperative management and antibiotics can be the treatment of choice. Mengoli and Klassen10documented this form of treatment in a series of 21 patients with thoracic esophageal perforations and pleural contamination. Eighteen patients were managed without thoracotomy with only a 6% mortality.10Also in these early years, Lyons et al compared results of the treatment of 18 patients with esophageal perforation with 11 patients managed without thoracotomy.11Mortality was 38% in the surgically treated group and only 9% in the conservatively managed patients.11As discussed by Cameron et al,9most of these patients did not have simply a contained perforation and chest tube drainage was used for free pleural fluid.9–11In a more recent review, Martinez et al reported successful “aggressive conservative” treatment in a series of iatrogenic perforations with 100% survival.12These authors suggested that perforations and pleural contamination, once controlled by adequate drainage, simply become an esophagocutaneous fistula (via the chest tube) and will heal similar to most gastrointestinal fistulas. We tend to agree with this hypothesis, and it has become the basis for our own institutional bias toward aggressive but nonoperative treatment of thoracic perforations.
How many cervical perforations require chest tube drainage?
None of the 10 cervical perforations required chest tube drainage. Of the 37 remaining esophageal perforations, chest tubes were placed in a total of 28 patients. Many patients had multiple chest tubes placed either bilaterally or on one side. Nine patients with iatrogenic perforations were treated with antibiotics and nasogastric and/or nasoesophageal intubation. Radiologic “pigtail” catheters or Thal Quik tubes were placed in addition to standard chest tubes in 6 patients with spontaneous perforation and 1 patient with an iatrogenic injury.
How long is a hospitalization for iatrogenic perforation?
Total hospitalization in the entire group (excluding the death on day 1) ranged from 3 to 90 days with a mean hospitalization of 25.9 days. The mean hospitalization in the 25 patients with iatrogenic perforation was 14.8 days (range, 3–46 days). The 14 patients with spontaneous perforation had an average hospitalization of 41 days (range, 14–90 days excluding the one death).
What are the measures of outcome in a perforation?
Measures of outcome include mortality, length of hospitalization, and esophageal healing.
How many patients survived esophageal perforation?
In summary, there was an overall survival of 96% in a total group of 47 patients presenting with esophageal perforations. Of the 32 patients treated nonoperatively, there was 100% survival. Esophageal healing occurred in 43 of 45 (96%) patients. Even in the patients with spontaneous esophageal disruption, 13 of 14 patients survived (93%).
How many patients were treated for a dissecting thoracic aortic aneurysm?
The 3 patients with dissecting thoracic aortic aneurysms were operated on for surgical repair of the dissection. Esophageal perforation was suspected in 2 patients. Two patients with esophageal tears underwent “patching” and extensive drainage. One healed primarily and the second healed following several weeks of adequate drainage. The third patient underwent esophageal exclusion by stapling and subsequently had a cervical esophagostomy. Following complete healing, this patient underwent a subsequent right colon interposition through the right anterior chest. All 3 patients survived aortic dissection and esophageal perforation.
How many patients were placed in a gastric tube?
Gastrostomy tubes were placed in a total of 8 patients (4 percutaneous and 4 operative with jejunostomy tubes). Three patients underwent separate placement of a jejunostomy tube during hospitalization. Most of the patients underwent parenteral hyperalimentation independent of the presence of G- or J-tubes.
Where is the proximal location of the esophagus?
proximal location is in the cervical esophagus at the
Can computed tomography show pleural?
and computed tomography of the chest can show pleural